The disease had been known for many years. When it made an appearance in a town or county, schools closed and children were kept away from each other, because catching this disease could mean debilitating long-term consequences and even death.
In the worst outbreak of the disease, over 58,000 cases were reported in the United States, mostly children though a third of the cases were in patients at least 15 years old. 36% of those who contracted the disease that year – over 21,000 – were left with permanent physical problems, including mild to complete paralysis. If the paralysis was focused on the chest muscles, patients could suffocate unless an apparatus to assist breathing, an iron lung, was available.
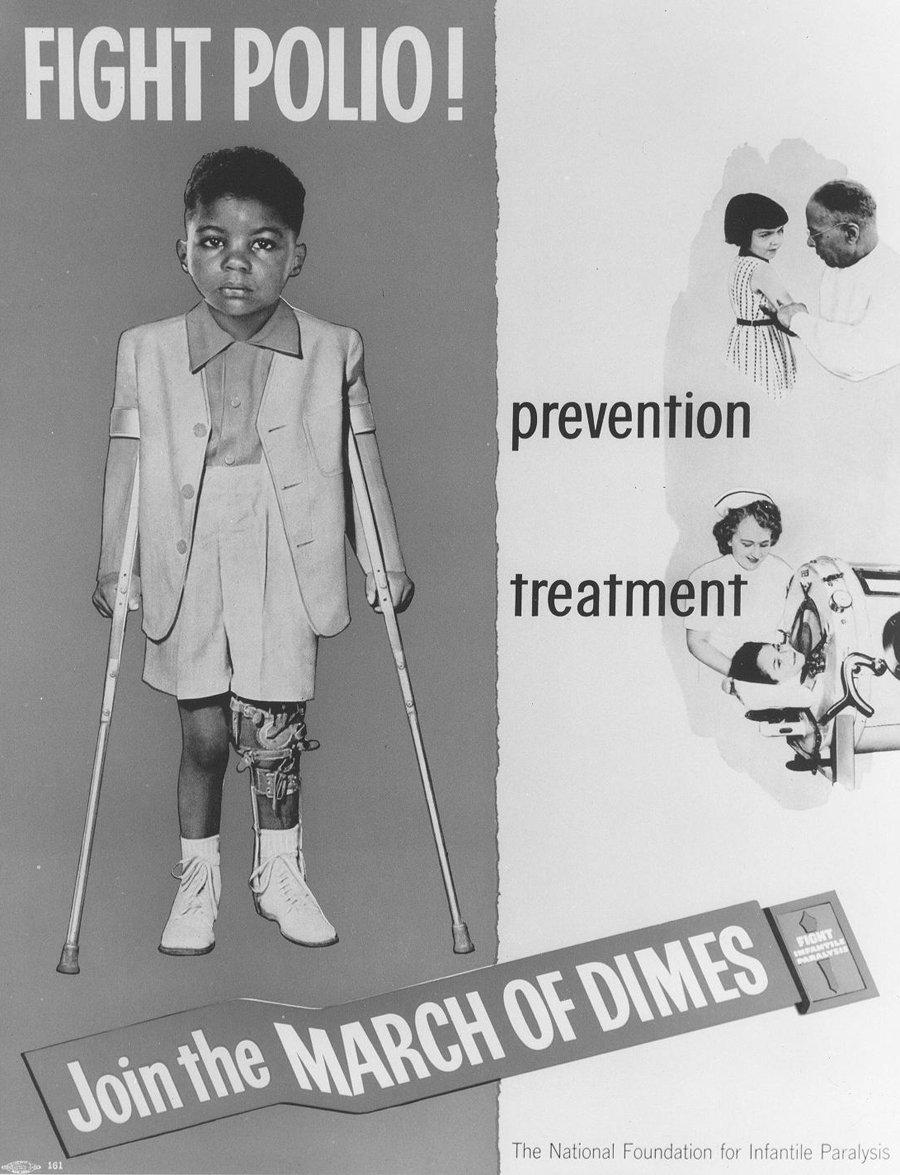
The disease was polio, and through a nationwide campaign to fund research into a vaccine (the March of Dimes) polio was eventually brought under control. The development of an inactivated polio virus vaccine by Jonas Salk in 1952 – the year of the worst polio epidemic in the U.S. history described above – and the oral attenuated virus vaccine developed by Albert Sabin in 1957 caused the number of polio cases in the U.S. and worldwide to rapidly decline. Today polio is considered eradicated in North and South America and only a handful of “wild” cases of polio (less than 200) were reported in 2019, mostly in Pakistan and Afghanistan.
While most children are vaccinated against polio, a growing number are not due to anti-vaccination campaigns throughout the U.S. and other western countries. We have a simple, inexpensive way to avoid the risks of polio, but some parents choose not to accept it for their children. There is no cure for polio. Most non-vaccinated people who contract polio (72%) have no symptoms, though long-term issues can occur. Another 24% have only mild illness from polio. But about 5 out of 1000 cases result in mild to severe paralysis which can result in death. Why take the risk?
We’re facing the same challenge in 2020, but the stakes are even higher. The peak number of polio cases in the U.S. was 58,000 in 1952; we already have over 7.7 million cases of COVID-19 in this country. In fact, yesterday (October 11) there were 46,069 new cases reported, nearly as many COVID-19 cases in one day as the total number of polio cases in 1952. We’ve had nearly 215,000 deaths that have been as a result of COVID-19 or significantly impacted by it. But despite having 132 times as many cases of COVID-19, we’re not working together to solve this pandemic. Large pharmaceutical companies, funded by various national governments, have stepped in and are racing to find a workable vaccine. Unfortunately, our other national pandemic – distrust in the government itself – threatens to undo any good that might come out of that work. In a recent CNN poll, only 51% of respondents said they would get the COVID-19 vaccine if one was available at low or no cost; 45% said they would not. (While there’s no evidence of correlation, it’s interesting that that’s about the same percentage of Americans who think Donald Trump is doing a good job as president.)
In Michigan, there’s an effort to pin blame on Gov. Gretchen Whitmer for the deaths of many elderly nursing home residents from COVID-19. 32% of the state’s deaths from COVID-19 lived in a nursing home. Certainly mistakes have been made as we’ve muddled through this crisis, but this blame game is led by the same people who either claim that the president has done a great job responding to coronavirus, wave the whole thing off as “fake news,” or both. Which is it? How can people die of something that’s fake?
If we can’t even agree that there’s a problem, how can we possibly come together to try to solve it?